Infection Prevention Orientation Manual
Section 18: Patient Engagement
Alicia Cole, BA – Communication; Alliance for Safety Awareness for Patients
October 2014
Download a printable PDF Version of this section.
Objectives
At the completion of this section the infection preventionist (IP) will learn:
- the benefits of effective communication for patient safety
- the five standards of effective communication
- some of the benefits to better communication
- some of the factors that contribute to communication failures in healthcare
- how emotions impact engagement and communication
- strategies for engagement
Number of hours
- All concepts – 1 hour
Overview
Patient engagement is a person’s sustained participation in managing their health in a way that creates the necessary self-efficacy to achieve physical, mental and social well-being. “Patient focus is something that needs to be welcomed, not discouraged,” says David Judge, MD, of Massachusetts General Hospital in Boston. Whether using simple techniques or complex technologies for patient engagement, healthcare providers must consider a patient’s social needs, and may need to weave more of that into care plans beyond the routine patient-physician visit. Patients who are conscious participants in their care and engaged by their providers have a better understanding of their condition and plan of care. This can lead to better compliance behaviors and medication adherence – increasing the likelihood of positive outcomes, lower readmissions, and higher patient satisfaction.
Key Concepts
Effective Communication for Patient Safety
Communication is when people exchange thoughts, messages, and information. It can be exchanged by speech, gestures, and writing. Effective communication is a two-way process that includes sending the right message that is also being correctly received and understood by the person/s on the other end. During the course of a 4-day hospital stay, a patient may interact with 50 different employees, including physicians, nurses, technicians, and others. Effective clinical practice involves many instances where critical information must be accurately communicated. Team collaboration is essential. When health care professionals are not communicating effectively, patient safety is at risk for several reasons: lack of critical information, misinterpretation of information, unclear orders over the telephone, and overlooked changes in status.¹ One study found that 93 percent of communication is affected more by our body language, attitude, and tone, than by the meaning and intent based on the actual words said (7 percent.)³ Whereas the spoken words contain the crucial content, their meaning can be influenced by the style of delivery, which includes the way speakers stand, speak, and look at a person.¹
Tips to ensure greater patient engagement and understanding:
- Have a face-to-face conversation with the patient to explain their condition. Use eye contact and speak concisely. Watch the client’s face and body language for reactions.
- Address the patient by using the correct salutation, such as Mr., Dr., Mrs. (i.e. some elderly patients state they feel disrespected when being addressed by their first name only.)
- Go down a list of important points for the patient to understand and check off each point after it has been discussed thoroughly. Make note of the patient’s concerns. Be sure to address them later. Handling all questions, no matter how small, makes the patient feel valued and at ease.
- Ask the patient or their family member if they would like additional literature on their condition. Share well-written materials such as brochures or computer printouts that explain their treatment and what they can expect.
Five Standards of Effective Communication
As with traditional business, applying the five standards of effective communication² to healthcare can facilitate improvements in the exchange of information between healthcare professionals and patients. These standards are listed and defined in Table 1.
Table 1. The five standards of effective communication and corresponding definition.
Benefits of Better Communication
The Joint Commission reports that investing in improving communication within the healthcare setting can lead to:
- Improved safety.
- Improved quality of care and patient outcomes.
- Decreased length of patient stay.
- Improved patient and family satisfaction.
- Enhanced staff morale and job satisfaction.⁴
Factors that Contribute to Communication Failures in Healthcare
The Joint Commission has reported the primary root cause of over 70 percent of sentinel events was communication failure.³ Breakdowns in healthcare communication are reported to occur due to:
- Human factors; attitudes, behaviors, morale, memory failures, stress and fatigue of staff
- Distractions and interruptions
- Shift changes
- Gender, social and cultural differences
- Hierarchy or power distance relationships (for example, junior staff are reluctant to report or question senior staff)
- Difference in training of doctors, nurses and paraprofessionals
- Time pressures and workload
- Limited ability to multitask even when highly skilled
- Lack of a shared mental model regarding what is to be achieved
- Lack of organization policies and/or protocols
- Organizational culture that discourages open communication
- Lack of defined roles and responsibilities among members of multidisciplinary teams.⁵
Emotions and their Impact on Engagement and Communication
When a patient is told, “You have an infection (or complication),” the diagnosis affects not only them, but also their family and friends who are caregivers. There are many emotions which can surface that may impact their ability to hear, process, communicate and engage effectively with their provider at that time. The patient and family may feel scared, uncertain, or angry about the unexpected complication. They immediately begin to have concerns about mortality, additional days of care leading to additional time off work, and consequences to their finances. Many patients will have to explain unexpected problems to children or concerned family members in other cities waiting to hear “everything is fine.” It can lead to a great deal of unexpressed anxiety and stress for a patient to handle.
It is imperative to understand how these emotions can affect the communication process and create barriers between care providers and their charge. While the healthcare provider may feel that they are explaining a diagnosis effectively, it is important to remember that the patient may be feeling numb or confused. The patient may have trouble listening to, understanding, or remembering what people tell them during this time. This is especially true when the doctor first tells the patient that he/she has an infection that will extend their stay in the hospital. It’s not uncommon for people to shut down mentally once they hear the words “infection or complication.” Additionally, if a patient is unfortunate and their infection progresses to a critical state, pain killers and other medications may foster the inability to clearly comprehend what they are being told or asked. This is an important reason patient advocacy is key to bridging the gap in patient engagement. A healthcare provider may be dealing with a family member or friend acting on behalf of the patient at that point and it is important to respect and consider the delicate nature of their position and emotional state.
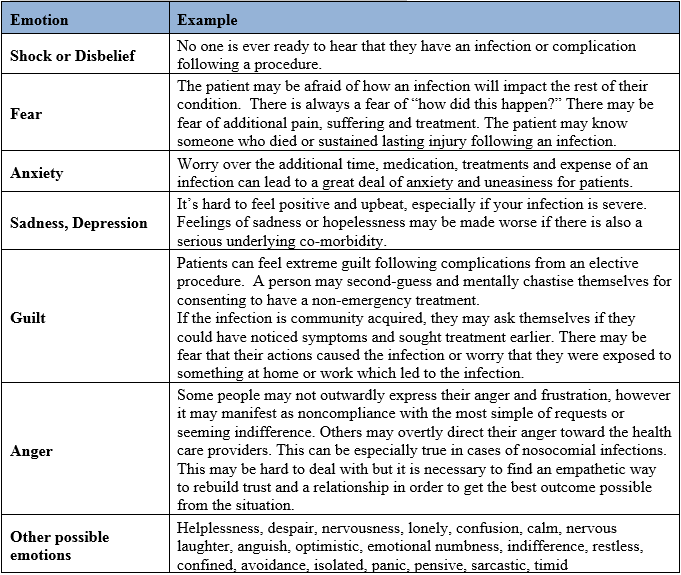
It is important to remember each person may have some or all of these feelings, and each will handle them in a different way. Strive to maintain good communication skills and not to take any emotional reactions personally. Emotions that patients may feel are listed and an example of each are provided in Table 2.
Table 2. Emotions patients may feel and an example of each.
Engagement Strategies
Numerous strategies exist to improve communication with patients and families. It’s important to find ones that work best for your facility and healthcare providers. No one strategy fits all situations and people.
Exercise
Pick 9 of the engagement strategies from the bank of examples below and give an example for how each may be used in your own practice.
Warm Greeting Limit Content Patient Participation
Complex Theory Indifference Impatience
Eye Contact Teach-back Plain, Non-Medical Language
Slow Down Repeat Key Points Confusion
Medical Jargon Avoidance Use Graphics When Explaining
Resources
Helpful Contacts
- Alicia Cole, Founder of Alliance for Safety Awareness for Patients (ASAP), 14622 Ventura Boulevard, #102-827, Sherman Oaks, CA 91403; 1-818-379-6979; https://www.patientsafetyasap.org/
Related Websites/Organizations
- Alliance for Safety Awareness for Patients (ASAP), https://www.patientsafetyasap.org/
- Mountain-Pacific Quality Health – Wyoming, https://www.mpqhf.com/wyoming/
- Healthcare Information and Management Systems Society (HIMSS) Center for Patient and Family-Centered Care, https://www.himss.org/NEHC
References
- Joint Commission on Accreditation of Healthcare Organizations.The Joint Commission guide to improving staff communication. Oakbrook Terrace, IL: Joint Commission Resources; 2005.
- The Joint Commission. 2007 National Patient Safety Goals. The Joint Commission, 2007.
- Allesandra T, O’Connor M.The platinum rule: discover the four basic business personalities and how they lead you to success.New York: Warner Books; 1966.
- Dunn, E.J., Mills, P.D., Neily, J., et al. (2007). Medical team training: applying crew resource management in the Veterans Health Administration. Jt Comm J Qual Patient Saf, 33(6): p. 317-25
- Murphy, H.A., Hildebrandt, H.W., and Thomas, J.P. Effective Business Communications. 7th ed. McGraw-Hill/Irwin. 1997.
- The Joint Commission. The Joint Commission Guide to Improving Staff Communication. Joint Commission on the Accreditation of Health Care Organizations. 2005
- Oandasan, I., Baker, G.R., Barker, K., et al. Teamwork in Healthcare: Promoting Effective Teamwork in Healthcare in Canada Canadian Health Research Foundation (CHSRF), June 2006.

WIPAG welcomes your comments and feedback on these sections.
For comments or inquiries, please contact:
Cody Loveland, MPH, Healthcare-Associated Infection (HAI) Prevention Coordinator
Infectious Disease Epidemiology Unit,
Public Health Sciences Section, Public Health Division
Wyoming Department of Health
6101 Yellowstone Road, Suite #510
Cheyenne, WY 82002
Tel: 307-777-8634 Fax: 307-777-5573
Email: cody.loveland@wyo.gov