Infection Prevention Orientation Manual
Section 7: Standard and Transmission-Based Precautions
Baerbel Merrill, MS, BSN, CIC
October, 2014
Download a printable PDF Version of this section.
Objectives
At the completion of this section the Infection Preventionist (IP) will:
- Understand the definition and use of standard precautions and transmission-based precautions
- Understand when standard and transmission-based precautions are to be applied to patients/residents in all healthcare settings
- Identify the key components of standard precautions and transmission-based precautions.
Number of hours
- Key Concepts – 4 hours
- Methods – 10 hours
Required Readings
- Healthcare Infection Control Practices Advisory Committee (HICPAC) 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Available at: cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf .
- World Health Organization: WHO Guidelines on Hand Hygiene in Health Car Available at: whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf .
- Grota P, Allen V, Boston KM, et al, eds. APIC Text of Infection Control & Epidemiolo 4th Edition. Washington, D.C.: Association for Professionals in Infection Control and Epidemiology, Inc.; 2014.
- Chapter 27, Hand Hygiene, by J Hass
- Chapter 28, Standard Precautions, by T Wiksten
- Chapter 29, Isolation Precaustions (Transmission-based Precautions), by C Berends and B Walesa
- Chapter 30, Aseptic Technique, by P Iwamoto and MT Post
Suggested Readings
- Bennett J and Brachman P, eds. Bennett & Brachman’s Hospital Infection 6th Edition. Philadelphia, PA: William R Jarvis; 2014.
- Chapter 43 Preventing Transmission of Bloodborne Pathogens in the Healthcare Setting, by DK Henderson
- Bennett G, Morrell G and Green L, eds. Infection Prevention Manual for Hospitals; revised edition. Rome, GA: ICP Associates, Inc.; 2010. Section 4: pages 1-59.
- Bennett G. Infection Prevention Manual for Ambulatory Care. Rome, GA: ICP Associates Inc.; 2009. Section 4: pages 1-46.
- Bennett G and Kassai M. Infection Prevention Manual for Ambulatory Surgery Centers. Rome, GA: ICP Associates, Inc.; 2011. Section 4: pages 1-54.
- Schweon S, Burdsall D, Hanchett M, et al. Infection Preventionist’s Guide to Long-Term Care. Washington, D.C.: Association for Professionals in Infection Control and Epidemiology, Inc.; 2013.
- Chapter 5, Isolation Precautions, by D Greene
Overview
Standard and transmission-based precautions are the cornerstone for all infection prevention activities to prevent healthcare-associated infections (HAI) and the transmission of communicable diseases to patients, staff and visitors. The materials in this chapter should be the foundation for all infection prevention and control activities. This information can be used to develop and review the policies and procedures implemented in a facility. The IP should also use this information to provide education to staff. Additionally, the IP will use this information for compliance review.
Key Concepts
The following information will include the principles of transmission of microorganisms and practices used to prevent the transmission of infection among patients and staff of and visitors to the healthcare facility.
Exercise #1
Review your institution’s current standard precautions and transmission-based precautions policies for compliance to the most current guidelines published by the Centers for Disease Control and Prevention (CDC) and the Association for Professionals in Infection Control and Epidemiology (APIC).
Chain of Infection
A break in the chain of infection can prevent the transmission of infection. Figure 1 provides a picture representation of the individual components of in the chain of infection.
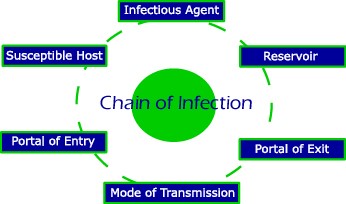
Figure 1. Chain of Infection. Adapted from RNCentral.com.
Infectious Agent:
An infectious agent is any disease-causing microorganism such as a bacterium, virus, parasite, or fungus. Characteristics of an disease-causing organism include the organism’s virulence (ability to multiply and grow), invasiveness (ability to enter tissue), and pathogenicity (ability to cause disease).
Reservoir:
A reservoir is the location or physical place that harbors microorganisms (pathogenic, opportunistic or non-pathogenic) and serves a possible source of infection. Reservoirs of disease can be inanimate such as toilet seats, elevator buttons, or animate such as food, water or human bodily fluids.
Portal of Exit:
The portal of exit is the physical location from which an organism leaves an animate reservoir, such as the respiratory tract (nose, mouth), intestinal tract (rectum), urinary tract, or blood and other body fluids.
Mode of Transmission:
The mode of transmission is the means by which an organism transfers from one carrier to another by either direct transmission (direct contact between infectious host and susceptible host) or indirect transmission (which involves an intermediate carrier like an environmental surface or a piece of equipment).
Portal of Entry:
The portal of entry is the physical location through which a pathogen enters the host’s body such as mucus membranes, open wounds, or tubes inserted in body cavities like urinary catheters, central lines or feeding tubes.
Susceptible Host:
A susceptible host is a person who is at risk for developing an infection. Several factors make a person more susceptible to disease including age (young people and elderly people generally are more at risk), underlying chronic diseases such as diabetes or asthma, conditions that weaken the immune system like HIV, certain types of medications, invasive devices like feeding tubes or central lines, and malnutrition.
Exercise #2
Sources/Reservoirs of Infection
The source and/or associated reservoirs of infectious agents are categorized into three distinct types: human, animal and environmental. It’s important for an IP to be aware of what the typical sources and reservoirs are of the common pathogens found in healthcare facilities in order to better control and prevent the spread of disease.
Exercise #3
Use the required and suggested readings to list example infectious agents for each source and reservoir: human, animal, environmental.
Routes of Transmission
The transmission of an infectious organism to a susceptible host occurs through three modes: direct or indirect contact (contact), droplets distributed in the air (droplet), and via the inhalation of air particles (airborne) which are generally smaller than droplets. The routes through which an infection can be spread is also important to both the IP and the HCP because each route will dictate the necessary personal protective equipment and precautions required to stop or inhibit that spread.
Exercise #4
Control Measures
Control of the transmission of infectious diseases is organized into three levels: 1) Engineering, 2) Administrative, and 3) Personal Protective Equipment.
Exercise #5
Use the required and suggested readings to provide the definition and an example of each of the listed categories of control measures in your facility: engineering, Administrative, Personal protective equipment (PPE).
Organizational, Administrative and Healthcare worker Responsibilities
When it comes to controlling and preventing the spread of infectious diseases within a healthcare facility, there are three levels of responsibility. This is similar to, and is in accordance with, the hierarchy of control measures. The first level of responsibility associated with control of disease transmission falls on the organization itself. The second level involves the facility’s or institution’s administration, and the third level relates to that of the healthcare worker.
In general, healthcare worker responsibilities for controlling and preventing the spread of disease occur through three activities (separately or in combination): 1) performing a point of care risk assessment (PCRA), 2) compliance with standard precautions, and 3) compliance with transmission-based precautions.
Exercise #6
Use the required and suggested readings, your facility policies, and interviews with your mentor/supervisor to provide an example of what your facility does to control/prevent transmission of infectious agents for each of the responsibilities listed.
- Organizational engineering control responsibilities
- Healthcare facility design, renovation, and construction; Heating, ventilation, and air conditioning; Source control
- Administrative control responsibilities
- Occupational Health, Education of staff, Repossessing of patient care equipment, Environmental Cleanup, Waste, Linen, Management of deceased patients/residents, Management of pets/animals
Exercise #7
Use the required and suggested readings, your facility policies, and interviews with your mentor/supervisor to define and give an example of each of the following healthcare worker responsibilities to control/prevent transmission of infectious agents: PCRA, Standard Precautions, Transmission-based Precautions.
Standard Precautions
Standard precautions are a group of infection prevention practices which include hand hygiene and the use of gloves, gowns, masks, eye protection or face shields depending on the anticipated exposure. The basic premise of standard precautions is to treat all patients’/residents’ blood or body fluid as if they are infectious. It is important to train all staff and monitor their compliance of these precautions. It’s recommended the IP aggregate reports of compliance to standard precautions policies and present the results to the facility’s Infection Prevention Committee.
The key components of both standard and transmission-based precautions include:
- Point of Care Risk Assessment
- Source Control
- Hand hygiene
- Patient Placement
- Patient Flow
- Aseptic Technique
- Personal Protective Equipment (PPE)
- Sharps Safety
- Visitor management
Point of Care Risk Assessment
Prior to every patient/resident interaction, all healthcare providers (HCPs) have the responsibility to assess the infectious risk posed to themselves, other HCPs, patients, or visitors. The ability to perform a thorough point of care risk assessment of the patient or resident and their environment is fundamental to practicing infection control. The IP needs to have a very complete understanding of how to do a risk assessment, how to include it in every patient/resident interaction, and how to use the findings to implement appropriate infection control practices (i.e., institution of standard and/or transmission-based precautions). The IP is required to educate healthcare providers about the point of care risk assessment and reinforce its use frequently. By applying the appropriate control measures as determined through the assessment, the healthcare provider can reduce the risk of infection to themselves, other healthcare staff, the patient/resident, and visitors.
Exercise #8
Exercise #9
Use the above information, and the required and suggested readings to complete Table 8. For each scenario pictured in the left most column, consider what questions would be asked during a PCRA and enter those in the middle column, entering infection control measures in the right most column. Note: the first scenario is an example. (Please download the printable PDF version of this section, linked at the top of the page, to view Table 8).
Source Control
Source control involves measures to separate those patients/residents with symptoms of various transmissible organisms from those without. These measures can include spatial separation whether in separate waiting rooms or the separation of patients by 2 meters for respiratory illnesses involving the production of aerosolized droplets (e.g., coughing). Other source control measures involve erecting partitions to protect staff, following facility specific protocol to place patients/residents with certain symptoms or known organisms directly into a single room. Options include placing patients with severe respiratory illnesses in negative pressure rooms if available. In certain settings, appointments can be made for these patients at the end of the day, or postponed until the acute phase of the illness has subsided. An IP should understand what supplies are necessary for source control in the facility. Such supplies include, but are not limited to: PPE, partitions, masks, etc. It is the institution’s responsibility to supply staff with the appropriate PPE.
Exercise #10
Hand Hygiene
Hand hygiene (HH) has been identified as the most effective way of preventing the transmission of healthcare-associated infection to patients, staff and visitors in all healthcare settings. Because HH represents a new term in the healthcare vocabulary it is critical that all infection control professionals become familiar with the new terminology and the heightened emphasis placed on HH in healthcare settings. Despite the fact that HH is considered the most important and most effective infection prevention and control measure, compliance with HH protocols by healthcare providers continues to be low. The five elements of HH that are important for every healthcare provider to understand are listed and described below:
- Indications for HH
- HH technique
- Agents used for HH
- HH policies
- HH compliance monitoring
Of particular importance to the IP are the facilities policies with regards to who, what, when and where HH should be performed, and monitoring the compliance with such policies. It is often the responsibility of the IP to perform audits of HH compliance.
Indications for Hand Hygiene
In every healthcare setting there are certain times that HH can and should be used for the best infection prevention. These select times are also referred to as “before” and “after” moments, and relate to before and after a healthcare provider will come in contact with a patient, resident or their environment.
Exercise #11
Use the required/suggested readings to list 5 before and after moments in healthcare in which hand hygiene must be performed.
Hand Hygiene Technique
Correct technique is a fundamental part of HH. There are many things to consider with regard to the correct performance of hand hygiene. These include the duration, hand characteristics (e.g., nail length), types of clothing and accessories worn, and areas of the hands that are often missed. Furthermore, there are two available methods for performing hand hygiene which have strengths and limitations.
Exercise #12
Exercise #13
List the strengths and limitations for both alcohol-based hand rub and traditional soap and water for performing hand hygiene.
Hand Hygiene Agents
A multitude of agents are available for HH in any healthcare facility type. The agent used in a particular location may depend on facility policy, price, staff acceptance, type of care performed in the setting, etc.
Exercise #14
Take a tour of the various locations, wards, units, or areas in your facility. Complete Table 13 by reviewing the hand hygiene agents currently in use in each of the areas or on a facility wide basis. You can choose which areas to designate as #1-5 and add more if necessary. Be sure to write the name of the area you designate as #1-5.
It may be a good idea to speak with the manager of each area to determine who is responsible for choosing and employing the HH agent for that specific area.
Is the IP staff involved with the tendering process for the hand hygiene agents?
(Please download the printable PDF version of this section, linked at the top of the page, to view Table 13)
Hand Hygiene Policy
Every healthcare facility should have a HH policy in place. There may be multiple policies in place that describe different aspects of HH, such as selecting the agents that will be used, or who is responsible for monitoring compliance. Additionally, there may be policies for each individual location within a healthcare facility. It is very important that the IP is familiar with all policies that relate to hand hygiene within their facility.
Exercise #15
Review your facility’s hand hygiene policy(s). Complete Table 14 by answering the questions as best as possible. (Please download the printable PDF version of this section, linked at the top of the page, to view Table 13)
Hand Hygiene Monitoring
As mentioned before, it is often the responsibility of the IP to monitor for compliance with hand hygiene policies and procedures. It is imperative for the IP to understand the audit process, why it’s important, and to whom, how and when the audit results are provided.
Exercise #16
Review your facility’s hand hygiene audit process and discuss with your supervisor or IP mentor.
- Is there a hand hygiene audit process for your facility?
- Who conducts the audits?
- Is there an education session for persons conducting the audit?
- Identify the methods used for collecting data to evaluate compliance?
- Who analyzes the data from the audits?
- How are the audits reported?
- Are staff provided with feedback from the audits?
- Who is responsible for implementing any changes recommended by the audits?
Patient Placement
Single rooms have been shown to lower healthcare-associated infections. When there are a limited number of single rooms available, it is prudent to prioritize them for those who have conditions that facilitate transmission of infectious material to other persons (e.g., draining wounds, stool incontinence, and uncontained secretions). Additionally, those patients/residents whom are at an increased risk of acquisition and adverse outcomes resulting from healthcare-associated infections (e.g., immuno-suppression, open wounds, indwelling catheters) should be placed in single/private rooms when possible.
Patient Flow
Patient flow refers to the transfer or transportation of patients/residents either within or outside of the facility, as well as individual patient/resident movement. It is necessary to use appropriate precautions when transporting patients/residents.
Exercise #17
Use the required/suggested readings, and the review your facility’s related policy(s) (i.e. patient transportation, HH, precautions, etc.) to describe the recommendation for transfer/transport of a patient/resident under the listed precaution both within and outside of your facility: Airborne precautions, droplet precautions, contact precautions.
Aseptic Techniques
Medical and laboratory procedures of any kind are performed under certain conditions and using one of two techniques: aseptic vs. clean. An awareness and understanding of each will help the IP to distinguish between the two techniques, know when aseptic technique is required and when clean technique is acceptable.
Exercise #18
Personal Protective Equipment
Personal protective equipment (PPE) is any type of specialized clothing, barrier product, or respiratory device used to protect the individual from potentially infectious persons, bodily fluids and excretions or contaminated objects. PPE acts as a barrier between infectious materials and the skin, mouth, nose, or eyes (mucous membranes). The routine use of PPE is an institutional requirement in all healthcare facilities. It is important for the IP and healthcare providers to understand the specific technique in which PPE is put on (don) and taken off (doff). Please see appendices A and B for pictures and to learn how to don and doff PPE. The three categories of PPE are:
- Gloves
- Gowns
- Facial protection (e.g. surgical masks or respirators)
Exercise #19
Use the required and suggested readings to complete Table 18. (Please download the printable PDF version of this section, linked at the top of the page, to view Table 13)
Sharp Safety and Prevention of Bloodborne Pathogens
Another critical element to consider for both standard and transmission based-precautions is sharp safety and the prevention of bloodborne pathogens.
Exercise #20
Use the required, suggested readings, and a review of your facility’s policies to answer the following questions:
- Define ‘sharp safety’.
- Name two precautions for handling sharps.
- What is your institutions policy on sharp safety?
- What are your sharps disposal units and where are they?
- Who disposes full sharps container?
- How often are staff members receiving education regarding sharp safety?
- What is the process to report sharp injury?
- Review your institutions blood and body fluid exposure policy. What are the critical elements and precautions mentioned?
Visitor Management
Visitor management is the control of both access and actions of people visiting patients/residents for the safety, security and prevention of disease transmission. It is also an important topic for review and consideration in terms of the implementation of and compliance with precautions.
Exercise #21
Review your institutions policy on visitor restrictions and answer the following questions:
- How are visitors alerted regarding precautions?
- Who provides the visitors with education regarding hand hygiene and the use of any required precautions (i.e. the use of PPE)?
- Is there a process for reviewing the visitors’ practices of hand hygiene and PPE to determine if it is being done properly? Who is responsible for this?
Transmission-Based Precautions:
Standard precautions, when applied correctly and consistently, will decrease the chance of transmitting of the majority of infections. However, there are other situations which will require targeted precautions to protect the patient, healthcare provider, visitor and the environment. These additional precautions are known as Transmission-Based Precautions and include:
- Contact Precautions
- Droplet Precautions
- Airborne Precautions
Contact Precautions
Contact precautions prevent the spread of infectious agents by direct and indirect contact. Key components of contact precautions include HH, PPE, patient placement, equipment management, patient transport, and visitor management.
Exercise #22
Exercise #23
List the type of precaution used and the duration for the following infections/conditions:
- Abscess, major, no dressing or dressing does not contain the drainage
- Diarrhea, acute, infective etiology suspected
- Antibiotic resistant organisms (e.g. MRSA, VRE)
- Clostridium difficile infection
Patient Placement for Contact Precautions
Although a private room with a dedicated bathroom is preferred for patients/residents under contact precautions, it is not always possible. If a private room is not possible, there are certain interventions that must be followed to cohort patients/residents.
Exercise #24
Droplet Precautions
Droplet precautions are used to interrupt the transmission of infectious agents that are spread by the droplet route. Similar to contact precautions, the key components to droplet precautions include: HH, PPE, patient placement, equipment, patient transportation, and visitor management.
Exercise #25
Use the required and suggested readings to answer the questions below.
- How are respiratory droplets generated?
- What is the area of defined risk for transmission of droplet particles?
Exercise #26
Patient Placement for Droplet Precautions
Again, a private room is recommended for patients/residents requiring droplet precautions. However, when this isn’t possible and cohorting patients/residents is necessary.
Exercise #27
For each of the following criteria, list important considerations for cohorting patients/residents under droplet precautions: Roommate conditions, Distance between patients, Privacy curtains .
Airborne Precautions
Airborne precautions are used to prevent the transmission of infectious agents that are spread through the air. This is different than droplet in the size of the particle and length of time they remain in aerosolized form. Similar to contact and droplet precautions, the key components of airborne precautions include: HH, PPE, patient placement, equipment, patient transportation, and visitor management.
Exercise #28
Use the required and suggested readings to answer the questions below.
- How are airborne particles generated?
- What is the area of defined risk for transmission of airborne particles?
Exercise #29
For each of the following infections spread by the airborne route, describe the type and duration of precautions used to prevent transmission of each: Tuberculosis, Varicella, Novel Respiratory Virus.
Exercise #30
Answer the following questions on topics in respirator use for the prevention of diseases transmitted through the airborne route:
- When is a respirator use required?
- What is the difference between a mask (surgical/procedure) and a respirator?
- Is there a Respiratory Protection Program in your facility?
- Have you been fit tested for a respirator?
- What is a fit check?
- Has the staff with patient/resident contact been fit tested?
- When was the last fit testing on N95 masks done at your facility?
Patient Placement for Airborne Precautions
Unlike both contact and droplet precautions, a private room with negative pressure is necessary, but it is not always possible.
Exercise #31
Immunization Status of Healthcare Worker Staff:
The PPE required to care for someone on airborne precautions depends on the staff member’s immunization status against the organism(s) involved (e.g., measles, varicella). However there are some airborne organisms against which a person cannot be immunized such as those that cause tuberculosis (TB) and severe acute respiratory syndrome (SARS).
Exercise #32
Other Issues
Aerosol Generating Procedures (AGP)
An aerosol generating procedure (AGP) is a medical or surgical procedure that may generate aerosols such as those performed during surgery, respiratory treatments, and suctioning. Examples of aerosol generating procedures include (but are not limited to):
- Elective intubation and extubation
- Bronchoscopy
- Sputum induction
- Autopsies
- Some procedures that occur in emergency situations such as cardiopulmonary resuscitation (CPR), emergent intubations and open suctioning of airways
It is prudent to avoid performing AGPs on a patient with known or suspected respiratory infection unless medically necessary. Until the infectious disease is resolved, either delay the procedure (if clinically appropriate) or make procedural changes to the care performed to reduce the risk of disease transmission. An example of a procedural change in this instance would be to use an aero chamber instead of a compressor to deliver aerosolized medications. Anytime a planned or emergent AGP must be performed on a patient/resident with a known or suspected respiratory illness, the use of a negative pressure room is recommended. Additionally, only those healthcare workers essential to performing the procedure should be in the room. In all circumstances, healthcare providers should wear a surgical mask and eye protection at a minimum. The use of an N95 mask or positive airway pressure Respirator (PAPR) is required when SARS, TB, or other emerging pathogens are suspected until the disease causing organism has been identified.
Exercise #33
Answer the following questions regarding AGPs:
- Define aerosol generating medical procedure
- Give 3 examples of procedures that are aerosol generating
- Give an example of how to avoid generating aerosol
- List the environmental controls that should be used for AGPs
- List some situations when to the use of an N95 mask or PAPR is required
- List the PPE that should be worn for a typical AGP
Handling of Deceased Bodies
Informing both healthcare providers and those who handle, transport and process deceased bodies of the necessary precautions is often a role IPs must take to prevent transmission of infectious and communicable diseases. The responsibility of notifying funeral home staff, morticians and/or coroners regarding an infectious disease or communicable illness of the deceased can also fall on the shoulders of an IP. It is important for an IP to be aware of their facility’s policies and local jurisdictions regulations or rules surrounding deceased bodies.
Exercise #34
Review your facility’s policies regarding the handling of deceased bodies. Determine who is responsible for notifying the funeral home, mortician, or coroner regarding any infectious disease the patient/resident had prior to death and the documentation necessary.
Determine if your county or local jurisdiction has a regulation regarding this situation.
Handling of Linen, Waste, Dishes and Cutlery
Healthcare facility staff members who handle linen, waste, dishes and cutlery are also at risk of acquiring infectious diseases and, as such, require some form of PPE. It is often the responsibility of the IP to review policies for the protection of these workers with regards to standard and transmission-based precautions and to institute a monitoring program to determine compliance.
Exercise #35
Review the “Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings 2007” as mentioned in the list of required readings. Describe the recommended precautions for healthcare worker staff for each of the following healthcare worker duties: Handling linen, handling hazardous waste, handling non-hazardous waste, Handling dishes, Handling cutlery.
Documentation and Reporting
There is no standard recommendation for the documentation of infection prevention and control activities in relation to specific patients or to specific groups. However, there are three good reasons to document the appropriate use of, and compliance with, policies related to standard and transmission-based precautions.
1. To facilitate communication
Through documentation, nurses communicate to other nurses and care providers their assessments about the status of clients, nursing interventions that are carried out, and the results of these interventions. Documentation of this information increases the likelihood that the client will receive consistent and informed care or service. Thorough, accurate documentation decreases the potential for miscommunication and errors. While documentation is most often done by nurses and care providers, there are situations where the client and family may document observations or care provided in order to communicate the information with members of the healthcare team.
2. To promote good nursing care
Documentation encourages nurses to assess client progress and determine which interventions are effective or ineffective, and identify and document changes to the plan of care as needed. Documentation can be a valuable source of data for making decisions about funding and resource management or to facilitate nursing research. These have the potential to improve the quality of nursing practice and client care. Individual nurses can use outcome information or critical incident to reflect on their practice and make needed changes based on evidence.
3. To meet professional and legal standards
Documentation is a valuable method for demonstrating that, within the nurse-patient relationship, the nurse has applied nursing knowledge, skills and judgment according to professional standards. The nurse’s documentation may be used as evidence in legal proceedings such as lawsuits, coroners’ inquests, and disciplinary hearings through professional regulatory bodies. In a court of law, the client’s health record serves as the legal record of the care or service provided. Nursing care and the documentation of that care will be measured according to the standard of reasonable and prudent nurse with similar education and experience in a similar situation.
Exercise #36
Resources
Helpful/Related Readings
- Heymann D. Control of Communicable Diseases Manual. 19th Washington, D.C.: American Public Health Association; 2008.
- Pickering L, et al, eds. Red Book: 2012 Report of the Committee on Infectious Diseases. 29th Elk Grove Village, IL: American Academy of Pediatrics; 2012.
- Mandell G, et al, eds. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 7th Edition. Philadelphia, PA: Churchill Livingstone Elsevier; 2010.
- Lautenbach E, Woeltje KF, and Malani PN, eds. SHEA Practical Healthcare Epidemiology (3rd Edition). University of Chicago Press, Chicago, IL; 2010
- Chapter 6 Isolation, by M Edmond and GML Bearman
- Chapter 21 Improving Hand Hygiene in Healthcare Settings, by JM Boyce and D Pittet
- Mayhall CG, ed. Hospital Epidemiology and Infection Control (4th Edition). Philadelphia, PA: Lippincott Williams & Wilkins, a Wolters Kluwer business; 2011.
- Chapter 90, Isolation of Patients with Communicable Diseases, by JE Bowling, J Cadena and JE Patterson
- Chapter 91, Hand Washing and Hand Disinfection, by ML Rotter
Helpful Contacts (in WY or US)
- Cody Loveland, MPH, Infectious Disease Surveillance Epidemiologist and HAI Prevention Coordinator, Wyoming Department of Health, 307-777-8634, cody.loveland@wyo.gov
- Baerbel Merrill, MS. BSN. CIC 307-689-3942 , michbaer@bresnan.net
Related Websites/Organizations
- Centers for Disease Control and Prevention: cdc.gov
- National Institute for Occupational Safety and Health: cdc.gov/niosh/
- U.S. Occupational Safety and Health Administration: www.osha.gov
- Wyoming Department of Health, Infectious Disease Epidemiology Unit, Healthcare-Associated Infection Prevention: https://www.health.wyo.gov/phsd/epiid/HAIgeneral.html
Appendices:
Please see the printable PDF version of this section to view the following appendices:
Appendix A: Proper sequence for Donning (putting on) of Personal Protective Equipment (PPE)
Appendix B: Proper sequence for Doffing (removal) of Personal Protective Equipment (PPE)

WIPAG welcomes your comments and feedback on these sections. For comments or inquiries, please contact:
Cody Loveland, MPH, Healthcare-Associated Infection (HAI) Prevention Coordinator
Infectious Disease Epidemiology Unit,
Public Health Sciences Section, Public Health Division
Wyoming Department of Health
6101 Yellowstone Road, Suite #510
Cheyenne, WY 82002
Tel: 307-777-8634 Fax: 307-777-5573
Email: cody.loveland@wyo.gov